This article first appeared in The Edge Malaysia Weekly on March 17, 2025 - March 23, 2025
IT has been five years since the Covid-19 pandemic began, but health experts say Malaysia could struggle to effectively deal with any similar outbreaks unless investments in pandemic preparedness are made. If followed through, however, such investments could put a strain on government finances, as no one knows when the next pandemic will be, they say.
Dr Muhammed Anis Abd Wahab, head of quality assurance at ProtectHealth Corp Sdn Bhd, a not-for-profit company under the Ministry of Health (MoH), thinks the country’s health system is not sufficiently prepared to handle another pandemic.
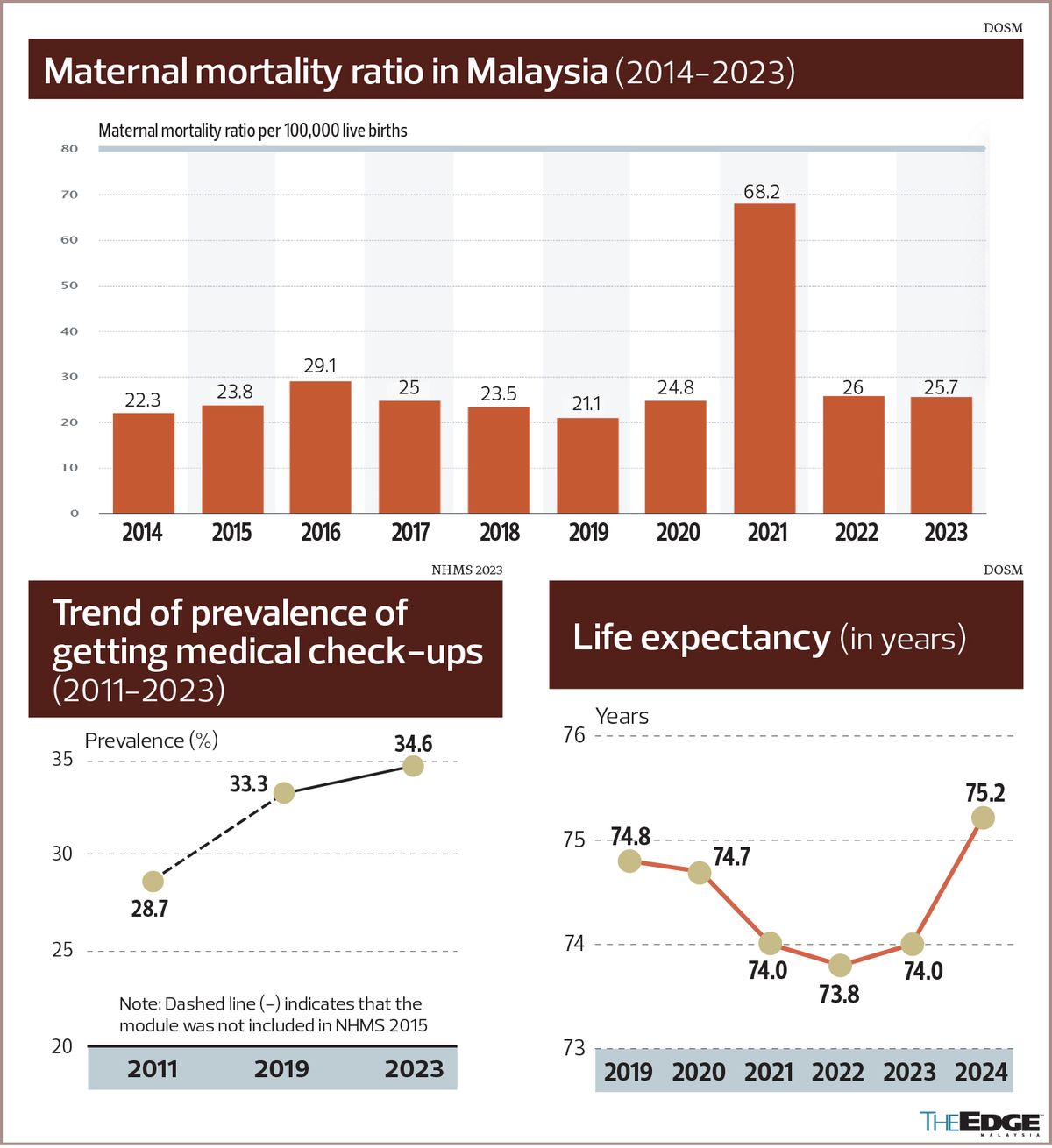
“This goes back to why we drafted the Health White Paper (HWP) for Malaysia [which was passed by Parliament in June 2023]. It was because we realised that our maternal mortality ratio (MMR) showed an increase during the pandemic. In 2021, the number of women who died during pregnancy or childbirth rose to 68.2 per 100,000 live births, compared with 24.8 in 2020. In 2022, the MMR had declined to 26, but was still higher than the rate in 2020.
“We were effective in reducing our MMR before the pandemic. When Covid-19 hit, however, we saw a dramatic rise in MMR, signalling that our health system wasn’t as strong as previously thought,” he tells The Edge in an interview.
“Maternal mortality” refers to deaths due to complications from pregnancy or childbirth.
More than 1½ years have lapsed since the 63-page HWP was passed, yet none of the proposed reforms to improve the Malaysian health system has been implemented.
The pandemic also caused life expectancy in Malaysia to fall between 2020 and 2022. Data from the Department of Statistics Malaysia (DOSM) shows that average life expectancy declined from 74.7 years in 2020 to 74 in 2021 and 73.8 in 2022. The good news is that life expectancy among Malaysians has improved, rising to 75.2 years last year from 74 in 2023.
“The HWP identifies that for Malaysia to be prepared for the next pandemic, we cannot work in a silo. It cannot just be an MoH initiative, that is, healthcare falls only under the ambit of MoH. It has to be a cross-society effort,” Muhammed Anis says, noting the importance of public-private partnerships (PPPs) during a pandemic.
In 2021, ProtectHealth was instrumental in getting private medical practitioners to participate in the National Covid-19 Immunisation Programme (PICK) after an initially slow rollout.
The company is also the administrator of the PeKa B40 scheme, an MoH initiative that offers free health services to the bottom 40% (B40) of income earners.
“Other agencies and non-health departments need to understand that the pandemic also had an impact on their livelihoods. If the government and non-government agencies work together and we have people understanding their role in promoting public health, then we will be ready [for the next pandemic],” Muhammed Anis adds.
He emphasises that although Malaysia remains vulnerable to another outbreak, the country is now better equipped to tackle it than it was five years ago.
“While things have improved, people still need to remember that it can always become worse if we are not prepared and do not build more resilience.”
Independent think tank Galen Centre for Health and Social Policy founder and CEO Azrul Mohd Khalib says it is “unfortunate” that Malaysians seem to want to forget the lessons from the pandemic, even pretending that it never happened, particularly in needing to protect vulnerable segments of the population such as the elderly, differently abled and infirm.
“Though systems that were developed during the pandemic, such as infectious disease surveillance, are in place, they may be inadequate if people themselves are not proactive in getting vaccinated against vaccine-preventable diseases such as influenza, Covid-19, dengue or even measles,” Azrul says in response to questions from The Edge.
Duopharma Biotech Bhd (KL:DPHARMA) group managing director Leonard Ariff Abdul Shatar concurs that the country is not ready for the next pandemic, but says no nation can be “100% ready”.
Taking the most recent pandemic as an example, he explains that when the World Health Organization raised the pandemic risk of Covid-19 to four on its five-stage system in 2020, Duopharma held an internal meeting among senior executives to anticipate what would happen in the event of a pandemic.
“We tried to second-guess what would happen during a pandemic and some of the decisions we made then have contributed to what we are still facing today. The first thing that we were concerned about was, if the pandemic closed down transportation lines, would we have sufficient raw materials for our production line? Generally, we keep four to six months’ worth of raw material inventory. But since we weren’t sure how long the pandemic would last, the first decision we made was to increase the amount of raw materials needed.
“So, throughout the 1½ years of the pandemic, we actually carried more stock than we would normally have done. Five years on, we’re [still] slowly normalising our stock levels,” says Leonard Ariff in an interview with The Edge.
As some countries grappled with a shortage of vitamin C during the pandemic, he points out that it was never an issue in Malaysia.
“This was primarily due to the [build-up of] stock that we acquired earlier,” he says.
The generic pharmaceutical group behind vitamin C brands such as Champs and Flavettes is the country’s largest supplier of the nutrient.
Lessons from Covid-19
Leonard Ariff says the pandemic has taught Duopharma that while the surge in demand for vitamin C benefited the country’s largest vitamin C producer, it also exposed the group to risks.
“When Malaysia entered the Covid-19 endemic phase in 2022, we saw a drop in demand for vitamin C. And every time we thought the fall had bottomed out, it fell further the following year,” he recalls.
He estimates that the group saw demand for its vitamin C plunge by 35% to 40% amid the transition from pandemic to an endemic phase. “It has taken us two years to work that [extra] stock through our system.”
Another lesson points to the importance of the country becoming self-reliant in developing and supplying its own critical drugs and vaccines, according to Leonard Ariff.
During the pandemic, Malaysia saw a shortage of various prescription and over-the-counter medications due to lockdown measures in China and the Russia-Ukraine war.
“How self-sufficient are we [in drug manufacturing] to cater for the next pandemic? The problem with a pandemic is that you never know whether it will be viral or microbial. So, you can’t invest to be totally pandemic-resilient. It doesn’t work that way,” he points out.
During the pandemic, communicating what people needed to know was another important lesson for the government.
“I hope MoH has learnt that just by keeping their frontliners — pharmacists and general practitioners — operating may not do the trick if people are afraid to leave their house [during a pandemic]. At the most, they’ll visit a government facility or a private hospital to seek first-line treatment. So, we must communicate to the public that going to their local pharmacy and clinic is perfectly safe,” he says, adding that the communication should include advice from MoH on ways people can protect themselves and prevent the spread of serious respiratory illnesses.
He points out that no country, including Malaysia, can be pandemic-proof.
“Rather, the question should be, what do we need to make us as resilient as possible to face the next pandemic? These include physical assets and manufacturing capabilities.
“Also, when it comes to the equipment needed by patients during a pandemic, how do we ensure that we are nimble enough to access additional quantities as and when it’s required? A pandemic response within Asean is worth thinking about,” he says.
While Malaysia had neither the capability or solution to produce vaccines for Covid-19, Leonard Ariff believes it still did “really well” in handling the health crisis.
“Malaysia is better prepared today than it was five years ago. Can we be better prepared? Yes, we can. But it depends on how much the government is prepared to lead a public-private initiative to address the next pandemic.”
Five years on, what has changed?
ProtectHealth’s Muhammed Anis says key findings from the National Health and Morbidity Survey (NHMS) 2023 revealed that the prevalence of medical check-ups showed an increasing trend with age.
“Among those who went for medical check-ups, one-third was self-initiated and almost all sought healthcare practitioners’ advice if there were abnormal findings, suggesting that our population is becoming more health literate.
“In addition, rural residents demonstrated a higher propensity to consult healthcare practitioners than their urban counterparts,” he says.
Still, health experts say most Malaysians have returned to life before the pandemic.
“Many people believe Covid-19 is over and that the disease is no longer a threat or even exists. This is reflected in issues such as attitudes towards healthcare and ageing,” says Galen Centre’s Azrul.
“However, medical practitioners in both public and private healthcare are observing that current hospital admissions seem to involve patients with much more severe illness for diseases such as respiratory disease, heart disease, chronic kidney disease, diabetes and even dengue. People are becoming more seriously ill, with a higher vulnerability towards longer hospitalisation, disability and premature death.
“As a result, more people are needing to be hospitalised, flooding public hospital emergency rooms and filling the wards of private hospitals. This has had a knock-on effect on demand for healthcare services such as health insurance utilisation, which has increased by more than 50%.
“Insurance premiums that were barely sufficient before are no longer adequate to provide adequate coverage, leading to changes and modifications in coverage (increase in co-payments and deductibles, and removal of cashless options).
“Malaysians appear to be more concerned about health, but are unlikely to invest more in healthcare because of the increasing unaffordability of private healthcare and health insurance,” he says, noting that the public healthcare system is expected to bear the brunt of this shift.
“People are also now more aware about vaccines than they were five years ago. Again, you have a minority who don’t believe vaccines help and a majority who believe that vaccines went some way towards ensuring that we came out of the pandemic well. The government was effective in vaccinating 80% of the population,” says Leonard Ariff.
“People are more attuned to the fact that if another pandemic occurs, there would have to be some form of vaccine as a first line of defence. From that perspective, people’s knowledge has improved,” he says. “However, whether Covid-19 has changed their lifestyles [and caused them to] become more health-conscious is something I don’t see at this stage.”
Read also:
Save by subscribing to us for your print and/or digital copy.
P/S: The Edge is also available on Apple's App Store and Android's Google Play.
- World Economic Forum highlights EPF as model for sustainable retirement reform
- Li Ka-shing's CK Hutchison mulls global telco assets spin-off, eyes London listing, Reuters reports
- U Mobile secures MCMC award, gears up for nationwide 5G roll-out
- Indonesians feeling market gloom ahead of major holiday
- Seeking opportunities in a risk-off market
- Trump pressing advisers for tariff escalation ahead of April 2, Washington Post reports
- Myanmar's quake toll passes 1,000 as extent of devastation emerges
- MetMalaysia can issue quake warnings within eight minutes, says DG
- Li Ka-shing's CK Hutchison mulls global telco assets spin-off, eyes London listing, Reuters reports
- Vance accuses Denmark of not keeping Greenland safe from Russia, China