THE Health White Paper (HWP) that was tabled in Parliament in June 2023 is an important document. Though short on specific details, it does give an indication of how the government intends to develop the national healthcare system.
There are several positive aspects to the HWP. Firstly, it is good to have a National Health Plan. And it is commendable that the government is inviting civil society to partake in the planning for our future healthcare needs. Most citizens will agree with the aspirations stated:
- building a healthy nation
- a healthcare system that:
- is equitable and affordable to the public
- is affordable to the nation and has sustainable financing
- makes use of the advances in digital technology
- optimises the use of all the healthcare resources both in the public and the private sectors.
The worrying aspect of the vision outlined in the HWP is that instead of setting out a series of incremental changes to the existing system, the HWP is advocating a major re-organisation of the Malaysian healthcare system as follows:
- The registration of all Malaysians under a primary healthcare clinic (PHC) of their choosing where they will get free treatment for minor illnesses and non-communicable diseases (NCDs).
- Free investigation and treatment in hospitals for patients with more serious complaints. However, to qualify for the free/subsidised treatment at hospital they need to be referred by their PHC. In effect, the PHC acts as a “gate-keeper” to further subsidised treatment.
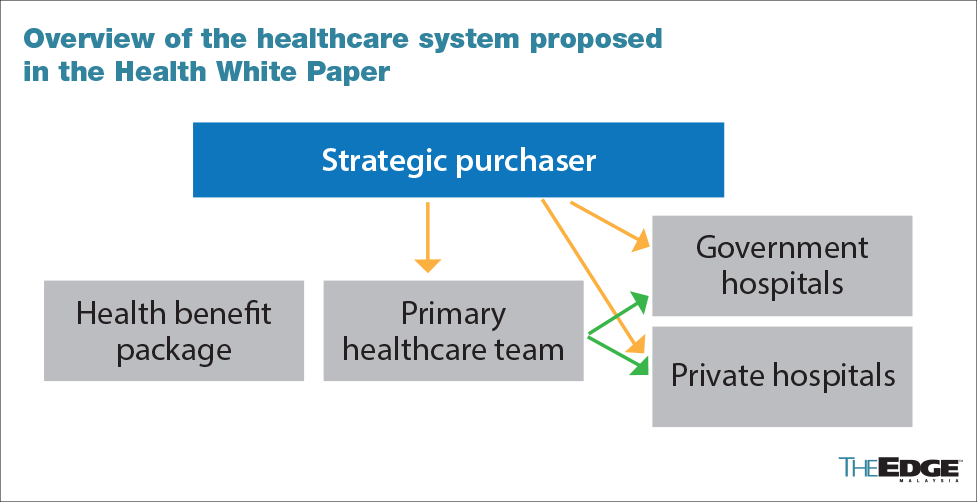
- The setting up of a “strategic purchaser” which is described as a not-for-profit entity that is separate from the Ministry of Health. The strategic purchaser will control most of the RM60 to RM80 billion fund allocated for the health sector each year. The strategic purchaser will pay PHCs, probably on a capitation basis, as well as the hospitals on the basis of investigations and treatment provided.
- Integration of private hospitals into the national healthcare system. This will be done by allowing PHCs to refer their patients to either government or private hospitals as the PHCs decide. A significant part of the charges in the private hospitals will be borne by the “strategic purchaser”.
The main features of the revamped healthcare system envisaged in the HWP is summarised in the chart below:
The HWP is advocating a major change in the financing of government hospitals. Currently, financial considerations are not the main drivers of clinical and administrative decisions in public hospitals. Switching to the strategic purchaser system where all hospitals are paid by the clinical services they provide will alter the way healthcare is delivered, in a fundamental way, and not necessarily for the better.
Medicine is not an exact science — the threshold for doing an appendectomy, or a caesarean section or a cardiac angiogram will be altered by financial considerations. The payment-for-services-provided system will create a tendency to over-investigate and to resort to surgery as these modalities will increase the revenue of the hospital. The overall cost of healthcare will then go up, because there will be financial incentives for hospitals to “over-investigate”, “over-diagnose” and “over-treat”.
The incidence of complications arising from medical interventions will also go up. The strategic purchaser will need to have a large army of employees to process claims from the various hospitals to ensure they are not over-claiming. This will also push up the cost of healthcare provision.
The HWP mentions “financial and operational autonomy for public sector providers”. Does this mean that public sector hospitals will be allowed to charge co-payments or offer services to health tourists to increase their incomes? If so, wouldn’t that lead to a disparity where public hospitals in poorer regions of the country have less revenue? Will the richer public sector hospitals be able to attract and retain more qualified staff compared to the poorer public sector hospitals in the rural areas and poorer states?
The aspirations stated in the HWP are impeccable. But attempting to attain these aspirations by “commodifying” healthcare and using market mechanisms may lead to perverse, unintended outcomes. And this is what we should try to avoid.
In the revamped system, the strategic purchaser will procure services in both the public and private sectors. This will essentially mean that a channel is provided for the public financing of the private healthcare sector. Will the diversion of public funds to private hospitals lead to the undermining of the public hospital system? It is important to remember the weaknesses of the private hospitals, which were not able to (or did not want to) manage Covid patients at the height of the pandemic. The Covid-19 pandemic showed very clearly that it is imperative to have a public healthcare sector that is strong and well-resourced in these times of emerging and re-emerging communicable diseases.
In the model outlined by the HWP, PHCs play a pivotal role in arranging care at the secondary and tertiary levels. Only patients referred by PHCs will get subsidised healthcare at the next level. The exact mechanism of the referral system is not as yet specified but is very important. If there are features — financial or otherwise — that penalise PHCs for referring too many patients to secondary or tertiary care, that could create a conflict of interest between PHCs and the patients under their care.
It is highly likely that private hospitals will try, by all means possible, to induce PHCs in their vicinity to refer patients requiring admission to them and not to public hospitals. Public hospitals would then be “defunded”.
So, yes, though the details are still to be provided, there are sufficient reasons for us to be concerned about the changes that have been outlined in the HWP. It is crucially important that civil society groups participate in any future consultations organised by the Ministry of Health to ask for details pertaining to the various proposals contained in the HWP and to give feedback.
The Peoples’ Health Forum’s suggestions for healthcare reform are as follows:
- Go for incremental changes — e.g. start a pilot project for some general practitioners (GPs) to be allocated NCD patients on a capitation basis. This will help decongest government clinics and personalise and improve care for NCDs. This can be expanded to other areas and more GPs if the pilot works well.
- Reduce wastages in the procurement of goods and services for public hospitals and clinics. The amount of mark-up that third party procurers can charge should be capped at a reasonable level.
- Increase the Ministry of Health budget to 4% of gross domestic product (GDP) in stages over five years.
- Make medium- and long-term plans to increase federal government revenue from its current 16.4% of GDP.
- Ensure that large commercial interests and professional groups that stand to gain financially from the further “commodification” of the Malaysian healthcare sector do not hijack efforts to improve healthcare for Malaysians.
Dr Jeyakumar Devaraj is the chairperson of the Socialist Party of Malaysia (PSM). He is a member of the People’s Health Forum (PHF). This commentary is the second in a series of three articles produced as a follow-up to the PHF’s Roundtable of Nov 7 to discuss the Ministry of Health’s Health White Paper.
- Former Petronas manager charged with disclosure of confidential information
- EcoWorld, SD Guthrie, NS Corp ink deal for joint venture to advance N Sembilan’s RM2.95b industrial park
- YTL Power unit wins bid to develop fibre optic along rail lines as RAC breaks industry monopoly
- Malaysia ready to develop Pan-Asian Railway Network — Loke
- Leapmotor’s Malaysian assembly plant to serve as Asean regional hub
- Trump studying whether to fire Fed chair Powell, adviser says
- White House seeks to bring financial regulators under its sway
- Capital One deal for Discover wins approval from US regulators
- Trump releases files on 1968 assassination of Robert F Kennedy
- China speeds up budget spending to counter tariff woes